Dental implants are one of the most effective solutions for replacing missing teeth, but they rely heavily on the health of your gums and jawbone. If you have gum problems such as periodontal disease, either currently or in the past, it’s natural to wonder whether you’re a candidate for implants. The truth is, gum disease doesn’t automatically disqualify you, but it does complicate the process. Both the presence of active infection and the long-term damage caused by previous periodontal issues can impact implant success. This post explains the key considerations, risks, and solutions if you’re thinking about getting dental implants with a history of gum disease.
What Is Periodontal Disease?
Periodontal disease, commonly known as gum disease, is a bacterial infection that affects the tissues supporting your teeth — primarily the gums and bone. It starts as gingivitis, a mild form that causes gum redness, swelling, and bleeding. If left untreated, it progresses to periodontitis, a more serious stage where the gums pull away from the teeth, forming pockets that trap bacteria.
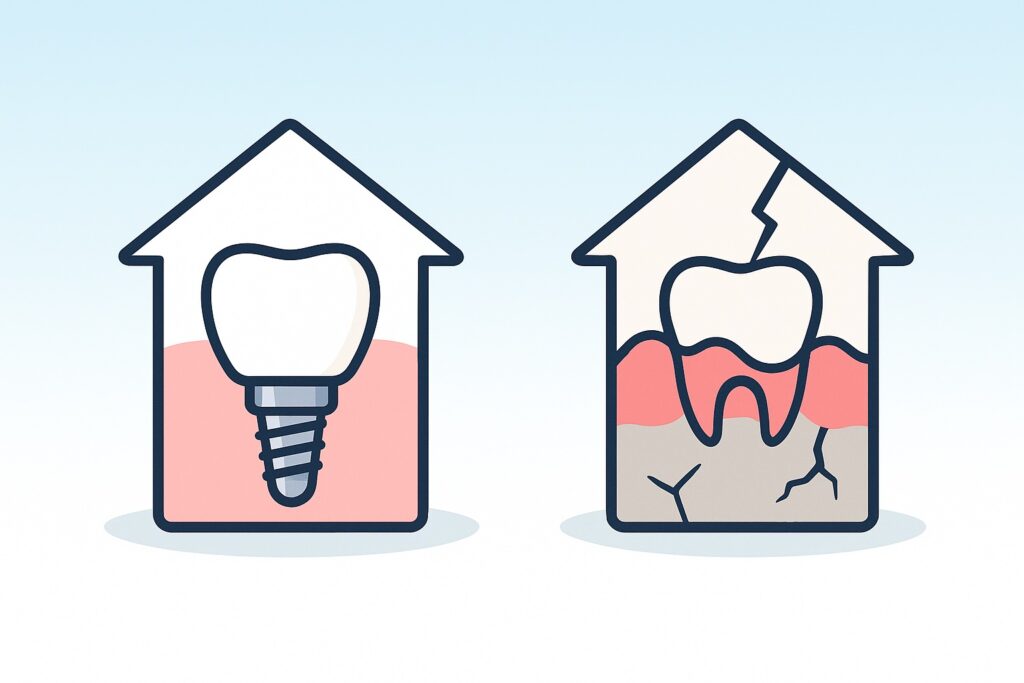
Over time, periodontitis can destroy the bone that holds your teeth in place, leading to tooth loss. This same bone is essential for supporting dental implants. Without healthy bone and gum tissue, implants cannot integrate properly with the jaw — a process called osseointegration. That’s why controlling gum disease is a critical first step before any implant procedure is considered.
Can You Get Implants with Active Periodontal Disease?
No — active periodontal disease must be treated before dental implants can be placed. The presence of ongoing infection poses a high risk of implant failure. Bacteria from untreated gums can spread to the implant site, causing inflammation around the implant known as peri-implantitis. This condition can lead to bone loss and eventual implant rejection.
Implants rely on stable, infection-free tissue to properly bond with the bone. If periodontitis is still active, your gums and bone are already compromised, making it impossible for the implant to heal and integrate successfully. Before moving forward, a periodontist or implant specialist will need to fully eliminate the infection, typically through deep cleaning (scaling and root planing), antibiotics, or surgical treatment if the disease is advanced.
Only after your gums are healthy and infection-free can implant planning begin.
What If You’ve Had Gum Disease in the Past?
Having a history of gum disease doesn’t automatically prevent you from getting dental implants — but it does mean you need a more cautious, customized treatment plan. If your periodontal disease has been successfully treated and your gums are currently stable, you may still be a good candidate.
Your dental team will assess several factors, including:
- Bone density and volume: Gum disease often leads to bone loss, which may require bone grafting before implant placement.
- Gum tissue health: Even in remission, weak or recessed gums can affect implant stability.
- Inflammation markers: Ongoing low-level inflammation, even without active disease, can increase the risk of complications.
The key is demonstrating a period of periodontal stability, usually verified through exams, probing depths, and x-rays. Regular dental cleanings and excellent oral hygiene habits are also essential before implants are considered. With proper preparation and monitoring, many patients with a history of gum disease successfully receive implants.
Risks of Getting Dental Implants with a History of Gum Problems
Even after successful treatment, having a history of gum disease increases the risk of complications with dental implants. Some of the most common concerns include:
1. Higher Risk of Peri-Implantitis
Peri-implantitis is an inflammatory condition affecting the tissues around an implant, similar to how periodontitis affects natural teeth. Patients with a history of gum disease are more prone to this condition, which can lead to bone loss and implant failure if not managed early.
2. Bone Loss Around the Implant
Previous periodontal disease may have already compromised the jawbone. Even after grafting, bone loss may continue over time if inflammation returns, threatening the long-term stability of the implant.
3. Slower Healing and Integration
Healing after implant placement can be slower in patients with a past of gum disease, especially if the immune system has been weakened or there’s residual inflammation in the tissues.
4. Increased Maintenance Needs
Implants in periodontally compromised mouths require more frequent dental visits and stricter oral hygiene routines to avoid reinfection.
While these risks don’t rule out implants entirely, they do require careful planning, monitoring, and a commitment to long-term maintenance.
Treatment Needed Before Implants Can Be Considered
If you have periodontal disease, your gums and bone must be restored to health before implant placement is an option. The exact treatment plan depends on how advanced the disease is, but the goal is to eliminate infection, stabilize the tissues, and rebuild any lost bone if needed.
1. Scaling and Root Planing
This deep cleaning procedure removes plaque and tartar from below the gumline and smooths root surfaces to help the gums reattach to the teeth. It’s the first line of treatment for moderate gum disease.
2. Antibiotic Therapy
Topical or oral antibiotics may be used alongside deep cleaning to reduce bacterial levels and inflammation.
3. Surgical Gum Treatment
In advanced cases, flap surgery or pocket reduction surgery may be needed to clean deep pockets and reshape the gum tissue for better healing.
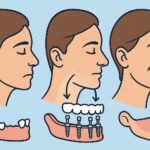
4. Bone Grafting
If gum disease has caused bone loss, a bone graft may be necessary to rebuild the jawbone before an implant can be placed. Grafting helps create a stable foundation for the implant post.
5. Healing and Monitoring
After treatment, your gums and bone need time to heal — often several months. Regular follow-up visits ensure that inflammation is gone, the bone is stable, and the mouth is ready for implant planning.
Starting implants before the disease is fully treated increases the chance of failure, so patience and proper treatment are essential.
How to Maintain Dental Implants if You’ve Had Gum Disease
Proper maintenance is critical to the long-term success of dental implants — especially for those with a history of gum disease. Even though implants aren’t natural teeth, they still rely on healthy gum and bone support, which means infection control remains a top priority.
1. Daily Oral Hygiene
Brush at least twice a day using a soft-bristle toothbrush and non-abrasive toothpaste. Floss daily or use interdental brushes to clean around the implant post, where plaque tends to accumulate.
2. Use Antibacterial Mouth Rinses
Your dentist may recommend an antimicrobial rinse (such as chlorhexidine) to reduce bacterial load and inflammation, particularly in the early months after implant placement.
3. Regular Periodontal Maintenance
After implants are placed, patients with a history of gum disease often require maintenance visits every 3–4 months. These visits include deep cleanings and monitoring for any signs of peri-implantitis or bone loss.
4. Avoid Smoking
Smoking significantly increases the risk of implant failure and worsens gum health. If you’re considering implants and have a history of periodontal issues, quitting smoking is strongly advised.
5. Watch for Warning Signs
Be alert to any bleeding, swelling, or discomfort around the implant site. Early detection of inflammation can prevent more serious complications.
Consistent care is what keeps implants healthy long-term — especially in patients more prone to gum-related issues.
Conclusion
Dental implants can still be a viable option if you’ve had gum problems — but only with proper treatment, careful planning, and long-term maintenance. Active periodontal disease must be fully addressed before any implant procedure begins, and those with a history of gum disease face higher risks that require closer monitoring. With the right care team and a strong commitment to oral hygiene, many patients with past gum issues successfully receive and maintain dental implants for years. The key is stability, both in gum health and bone support, before and after placement.