Dental implants have become the gold standard for replacing missing teeth due to their durability, functionality, and natural appearance. However, one of the most serious complications that can compromise an implant’s longevity is bone loss around the implant site. This bone resorption not only weakens the support structure but can ultimately lead to implant failure if not addressed in time.
Understanding the underlying causes of bone loss around implants is essential for both dental professionals and patients. From biological factors like inflammation to mechanical stress or surgical error, several variables can trigger this gradual degradation. Fortunately, many of these issues can be prevented or mitigated with proper planning, technique, and aftercare.
1. Peri-Implantitis: Inflammation-Induced Bone Loss
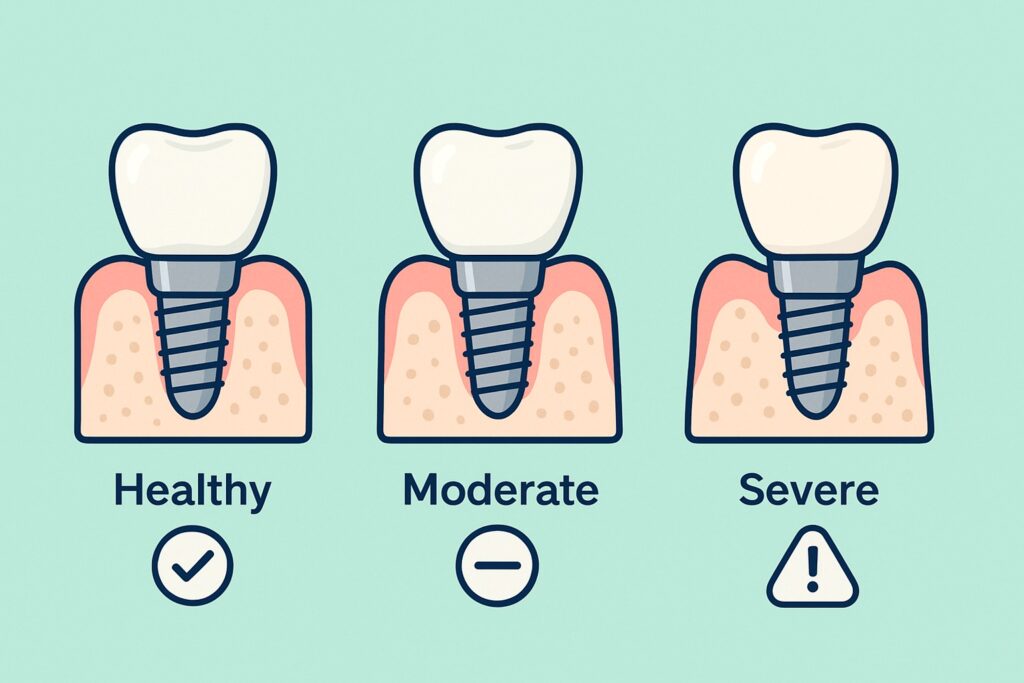
Peri-implantitis is one of the leading causes of bone loss around dental implants. It is an inflammatory condition affecting the soft and hard tissues surrounding an implant, similar in nature to periodontitis but specific to implants. If not diagnosed and treated early, peri-implantitis can result in progressive bone destruction and eventual implant failure.
The condition typically begins with the accumulation of bacterial plaque around the implant. When oral hygiene is poor or the implant surface is rough and difficult to clean, bacteria colonize the area and provoke an immune response. This leads to swelling, bleeding, and inflammation in the surrounding gum tissue. As the infection penetrates deeper, it starts breaking down the bone supporting the implant.
Early signs of peri-implantitis include bleeding on probing, pus discharge, increased pocket depth, and radiographic bone loss. Because the disease is often painless in the initial stages, it can go unnoticed until significant bone has already been lost.
Timely intervention is critical. Non-surgical treatments like scaling, antiseptics, and antibiotics may help in the early stages, while advanced cases may require surgical debridement or even implant removal.
2. Poor Implant Placement or Surgical Technique
Improper surgical technique or inaccurate implant positioning is another major contributor to bone loss. The precision required for successful implant placement is high, and even slight deviations can lead to biological or mechanical complications.
One common issue is placing the implant too close to adjacent teeth or other implants, which can restrict natural bone remodeling or compromise blood supply to the surrounding bone. Inadequate spacing can also prevent proper gum tissue adaptation, leading to persistent inflammation and eventual bone resorption.
Overheating the bone during drilling is another surgical risk. If proper irrigation is not maintained or the drilling speed is too high, thermal injury can occur, damaging bone cells and impairing osseointegration — the process by which the implant fuses with bone. This damage often leads to early implant failure or delayed bone loss.
Additionally, implants placed at incorrect angles or depths can create excessive stress on specific parts of the surrounding bone. These micromovements, especially during the healing phase, prevent stable integration and may cause bone to recede around the implant over time.
Using advanced imaging like CBCT scans, digital planning software, and surgical guides significantly reduces these risks. Skilled surgical execution, combined with thorough preoperative planning, is essential to preserving bone health around implants.
3. Overloading the Implant
Implant overloading occurs when excessive or uneven forces are applied to an implant, either too early during healing or due to improper prosthetic design. This mechanical stress can overwhelm the surrounding bone, leading to microfractures, bone fatigue, and eventual resorption.
One of the most common causes is premature loading — when a crown or bridge is attached to the implant before the bone has fully integrated. Although immediate loading is sometimes used in specific clinical cases, it requires ideal conditions such as high bone density and excellent initial implant stability. In less-than-optimal situations, early loading can disrupt osseointegration and trigger bone loss.
Occlusal overload, where biting forces are not evenly distributed across the dental arch, is another contributing factor. Poor alignment or prosthetic design may cause certain implants to bear more force than others, especially during chewing. This stress creates excessive pressure on the surrounding bone, compromising its ability to maintain structural integrity.
Nighttime clenching or grinding (bruxism) can further worsen this issue. If not identified and managed with night guards or occlusal adjustments, the repetitive pressure can cause gradual loss of bone even around otherwise well-integrated implants.
Proper load distribution, careful prosthetic planning, and ongoing monitoring are essential to prevent mechanical overload and preserve long-term implant success.
4. Systemic Health and Bone Metabolism Disorders
Systemic health conditions play a significant role in bone healing and maintenance around dental implants. Certain diseases and medications can interfere with bone metabolism, increase inflammation, or impair immune response — all of which can lead to accelerated bone loss.
Diabetes mellitus, particularly when poorly controlled, is a known risk factor. Elevated blood glucose levels compromise wound healing, reduce immune defense, and promote chronic inflammation. This creates a more favorable environment for infections like peri-implantitis and hinders proper osseointegration.
Osteoporosis is another major concern. In patients with low bone density, the jawbone may lack the structural strength needed to support an implant, increasing the risk of bone resorption. The use of medications like bisphosphonates or antiresorptive agents (commonly used to treat osteoporosis or cancer-related bone disease) can also interfere with normal bone remodeling and pose a risk for osteonecrosis, especially following surgical procedures.
Smoking significantly affects bone health as well. It reduces blood flow to the bone and soft tissues, delays healing, and impairs immune response — all contributing to a higher risk of implant complications, including bone loss.
Other health issues such as autoimmune diseases, hormonal imbalances, and immunosuppressive therapy may further reduce the body’s capacity to maintain healthy bone around implants.
Managing these risks involves comprehensive medical evaluation, pre-surgical planning, and close coordination between the dental provider and the patient’s physician. Patients with systemic conditions must be carefully monitored throughout the treatment and follow-up phases to ensure implant stability.
5. Lack of Initial Bone Volume or Grafting Failure
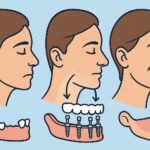
Sufficient bone volume is critical for the long-term success of dental implants. When implants are placed in areas with inadequate bone — either due to natural resorption after tooth loss, trauma, or periodontal disease — the risk of future bone loss increases significantly.
If an implant is inserted into compromised bone without prior augmentation, there may be insufficient support for proper osseointegration. Over time, this weak foundation can lead to implant instability and progressive bone resorption as the body attempts to adapt to the load and foreign material.
To address this, bone grafting procedures are often used to rebuild the site before or during implant placement. However, if the graft fails to integrate properly — due to infection, poor technique, or the patient’s medical condition — the site may still lack the structural integrity required to maintain the implant.
Additionally, even successful grafts can undergo some degree of resorption over time, especially if they were performed with poor-quality materials or in high-stress areas. This slow degradation can result in gradual loss of bone support and potential implant complications years after placement.
Ensuring proper case selection, using high-quality grafting materials, and allowing adequate healing time before implant placement are essential steps in reducing these risks. Post-operative monitoring through imaging can also help detect early signs of graft or implant failure.
6. Prevention Strategies and Long-Term Care
Preventing bone loss around dental implants starts well before the implant is placed and continues long after it has been restored. A proactive approach combining precise planning, surgical excellence, and patient compliance is key to ensuring long-term implant health.
Comprehensive pre-surgical evaluation is critical. Advanced imaging techniques such as CBCT scans help assess bone volume, density, and anatomical landmarks, allowing for accurate planning of implant size, angulation, and position. If bone is insufficient, grafting procedures should be performed in advance, with enough healing time to ensure success.
Proper surgical technique reduces trauma to the bone. Using sharp, sterile instruments, avoiding excessive heat during drilling, and maintaining primary stability without over-compression all contribute to better osseointegration and long-term bone preservation.
Once the implant is placed and restored, routine maintenance and monitoring become essential. Patients must be educated about meticulous oral hygiene practices to reduce bacterial load and prevent peri-implantitis. Professional cleanings, especially around implant-supported restorations, should be scheduled regularly.
Bite analysis is another critical aspect. Any signs of occlusal overload should be corrected through adjustments or the use of protective devices like night guards, especially in patients with bruxism. Ensuring the prosthesis is properly designed and aligned helps distribute forces evenly across the arch.
For patients with systemic conditions, close collaboration between the dental team and medical providers helps manage risk factors. Smoking cessation, blood sugar control, and monitoring of bone-affecting medications can significantly improve implant outcomes.
Ultimately, successful implant care is a shared responsibility. When patients are informed and engaged, and clinicians take a comprehensive approach, the chances of bone loss are greatly reduced.
Conclusion
Bone loss around dental implants is a complex issue with multiple contributing factors — from bacterial infection and surgical technique to systemic health and biomechanical stress. Left unaddressed, it can compromise the stability of the implant and lead to complete failure.
However, most causes of bone resorption are either preventable or manageable with the right protocols. Thorough planning, skilled execution, and consistent long-term maintenance are essential. Just as importantly, patient education and cooperation play a central role in minimizing risks and preserving the health of both the implant and surrounding bone.
With proper care, dental implants can provide a stable, long-lasting solution for tooth replacement — free from the complications of bone loss.