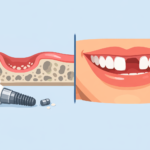
Dental implants might seem like a modern marvel, but they actually have a straightforward design. At their core, these implants are meant to replace missing teeth and help restore your smile. They’re made up of three key components that work together harmoniously.
The first part is the implant itself, which is usually a small titanium post surgically placed into the jawbone. Imagine it as the tooth root; it needs to integrate with your bone to provide stability. You might wonder if it hurts—most people report feeling surprised at how little discomfort there actually is due to the numbing process.
Next, there’s the abutment. Think of it as the connector that sits above the gum line. This piece holds the crown in place and is crucial for a natural look. It’s typically made of materials like titanium or ceramic, ensuring a strong yet aesthetic finish.
Last but not least, we have the crown, which is the visible part of the implant that mimics the shape and color of your natural teeth. It’s custom-made to fit your mouth perfectly, ensuring a blend with your existing smile.
So when you consider dental implants, it’s these three components that make it all come together—each one playing a vital role in restoring function and beauty to your smile.
H2 2: Key Components of Dental Implants
Dental implants are more than just small titanium posts that go into your jawbone; they’re a surprisingly intricate system designed to mimic the natural tooth structure. Let’s break down the key components you’ll find in most dental implants.
First off, there’s the implant itself, which is usually made of titanium due to its compatibility with the human body. This is the part that fuses with your jawbone through a process called osseointegration. It might sound a bit technical, but essentially, your bone grows around the implant, securing it in place. If you’ve ever had a tooth extracted, gap in your smile, or felt the difference of a lost tooth, you’ll understand how crucial this part is.
Next up, we have the abutment. This small connector piece sits on top of the implant and connects it to the crown, or the visible part of the tooth. Think of it as a bridge between the implant and the crown, providing stability. Choosing the right abutment is essential, as different shapes and sizes align better with different crowns.
Finally, there’s the crown itself, which can be made of various materials like porcelain or resin and is designed to look just like a natural tooth. It’s the part that not only restores function but also aesthetics—after all, nobody wants a tooth that looks out of place. Each of these components plays a vital role in ensuring that dental implants are functional, comfortable, and lifelike.
H2 3: Dental Implant Surgery Process
Getting a dental implant isn’t just about slapping a new tooth in your mouth. It’s a bit more involved, and understanding the surgery process can help ease your mind if you’re considering it. Typically, the procedure starts with a consultation where your dentist will evaluate your dental health and discuss what’s best for you.
On the actual day of surgery, you’ll likely be given some form of anesthesia. Most people feel more at ease knowing they won’t feel a thing during the process. Once you’re comfortable, the dentist will surgically place the implant into your jawbone; think of it as inserting a small screw. This is a vital step because it serves as the foundation for your new tooth. After that, it usually takes a few months for the bone to integrate with the implant, a process called osseointegration.
After healing, a small connector, called an abutment, is added, which will hold your artificial tooth in place. The final step is creating and securing the crown, which is the part people actually see. It’s a multi-step journey, but in the end, many find it’s well worth the effort for a restored smile.
H2 4: Cost Factors for Dental Implants
When considering dental implants, understanding the cost is crucial. It’s not just about the price of the implant itself; several factors play into the total you’ll end up paying. For one, the type of material used can vary. Titanium is a popular choice due to its strength and compatibility with bone, but it can be pricier than other options.
Another key factor is the complexity of your specific situation. If you have bone loss and need a bone graft before getting the implant, that’ll add to the overall cost. Even geographic location matters; dental services in urban areas often have higher labor and overhead costs than those in smaller towns.
- Consultation fees – Initial examinations and imaging can add more to the bill.
- Follow-up visits – Make sure to factor in post-operative care and maintenance.
- Insurance coverage – Some plans cover part of the cost, but it varies widely.
So, before diving in, it’s a good idea to chat with your dentist about all these elements and get a clear picture of what to expect financially.
H2 5: Common Mistakes to Avoid with Dental Implants
Getting dental implants can feel like a big step, and it’s easy to slip into some common pitfalls along the way. One major mistake is skimping on the aftercare. You might think once the implants are in, you can treat them like normal teeth, but that’s not quite right. Regular follow-ups with your dentist are crucial for ensuring everything’s healing properly.
Another issue is ignoring the role of good oral hygiene. Just because implants don’t decay like natural teeth doesn’t mean you can abandon brushing and flossing. If you let plaque build-up happen, you could risk infections or complications. You really want those implants to last a long time, so take care of your mouth like you would if they were your natural teeth.
- Don’t skip out on recommended follow-up visits.
- Make sure to maintain a solid oral hygiene routine.
- Avoid hard foods right after surgery; give your mouth some time to adjust.
H2 6: Maintenance and Care for Dental Implants
Taking care of your dental implants is crucial if you want them to last. Just like natural teeth, they need regular attention. Brushing twice a day and flossing regularly is non-negotiable. Use a soft-bristled toothbrush to avoid damaging the gum tissue around the implant.
It’s a good idea to steer clear of hard foods, at least in the beginning. Things you might normally crunch on, like ice or hard candies, can put unnecessary stress on your new teeth. And don’t forget about those dental check-ups! Regular visits to your dentist help catch any potential issues before they become a headache.
- Rinse with an antibacterial mouthwash to keep infections at bay.
- Consider using an interdental brush for those hard-to-reach spots.
- Be mindful of any discomfort or changes; they’re worth mentioning to your dentist right away.
H2 7: FAQs About Dental Implant Components
Got questions about the components of dental implants? You’re not alone! Here are some common queries people have:
- What’s the purpose of the abutment? The abutment serves as the connector between the implant and the crown. Think of it as the bridge that holds everything together.
- How does the implant integrate with the jawbone? The process is called osseointegration. Essentially, your jawbone grows around the implant, making it super secure. It’s like your body’s way of accepting the implant as part of itself.
- Can I get an implant if I have gum disease? It’s best to treat any gum disease first. Your dentist will likely recommend ensuring your gums are healthy before moving forward with implants.
- How long do implants last? With proper care, dental implants can last well over a decade, often much longer. Regular dental check-ups are key to their longevity.
If you have more specific questions, don’t hesitate to bring them up with your dentist. They can give you personalized insights based on your own dental health.
H2 8: How to Choose the Right Dental Implant Type
Choosing the right dental implant type can feel a bit overwhelming, but it doesn’t have to be. Start by considering your specific needs and lifestyle. Think about factors like how many teeth you’re missing and whether you have any underlying health issues that might complicate the process.
There are a few options available that cater to different situations:
- Endosteal implants: These are the most common type. They’re placed directly into the jawbone and are best suited for those with healthy jawbones.
- Subperiosteal implants: If you don’t have enough natural jawbone to support an endosteal implant, this alternative sits on top of the bone but under the gum tissue.
- Zygomatic implants: A less common choice, these are inserted into the cheekbone. They’re often used for patients with extreme bone loss.
Don’t forget to consult with your dentist or oral surgeon. They’ll walk you through the pros and cons of each type, helping you make a more informed decision. It’s all about finding what works best for you!
H2 9: Impact of Bone Density on Implant Success
Bone density plays a crucial role in the success of dental implants. If the bone isn’t dense or strong enough, the implant may not integrate properly, which can lead to complications down the line. Think of it like trying to anchor a tall flagpole in loose sandy soil—it’s just not going to have the support it needs.
A few factors can affect bone density. Age, for instance, can cause bone loss, especially in older adults. Also, conditions like osteoporosis can weaken bone structure, making it essential for your dentist to evaluate your bone health before proceeding with implants. Sometimes, a simple bone graft can provide the necessary support—essentially reinforcing that sandy soil so your flagpole stands tall.
- Prior dental extractions can impact density in that area.
- Smoking or certain medications may contribute to bone loss.