Choosing the right dental implant material goes beyond just biocompatibility. For dental professionals, understanding the composition, safety profile, and performance of materials like titanium and zirconia directly impacts clinical outcomes and long-term success rates. Titanium has long been the standard due to its proven track record in osseointegration and strength. However, zirconia has emerged as a viable metal-free alternative, offering improved aesthetics and favorable tissue response in select cases. The decision between the two is increasingly influenced by patient-specific factors, such as metal sensitivities, soft tissue behavior, and aesthetic demands, making material knowledge essential in practice.
Titanium Dental Implants
Composition and Types of Titanium Used
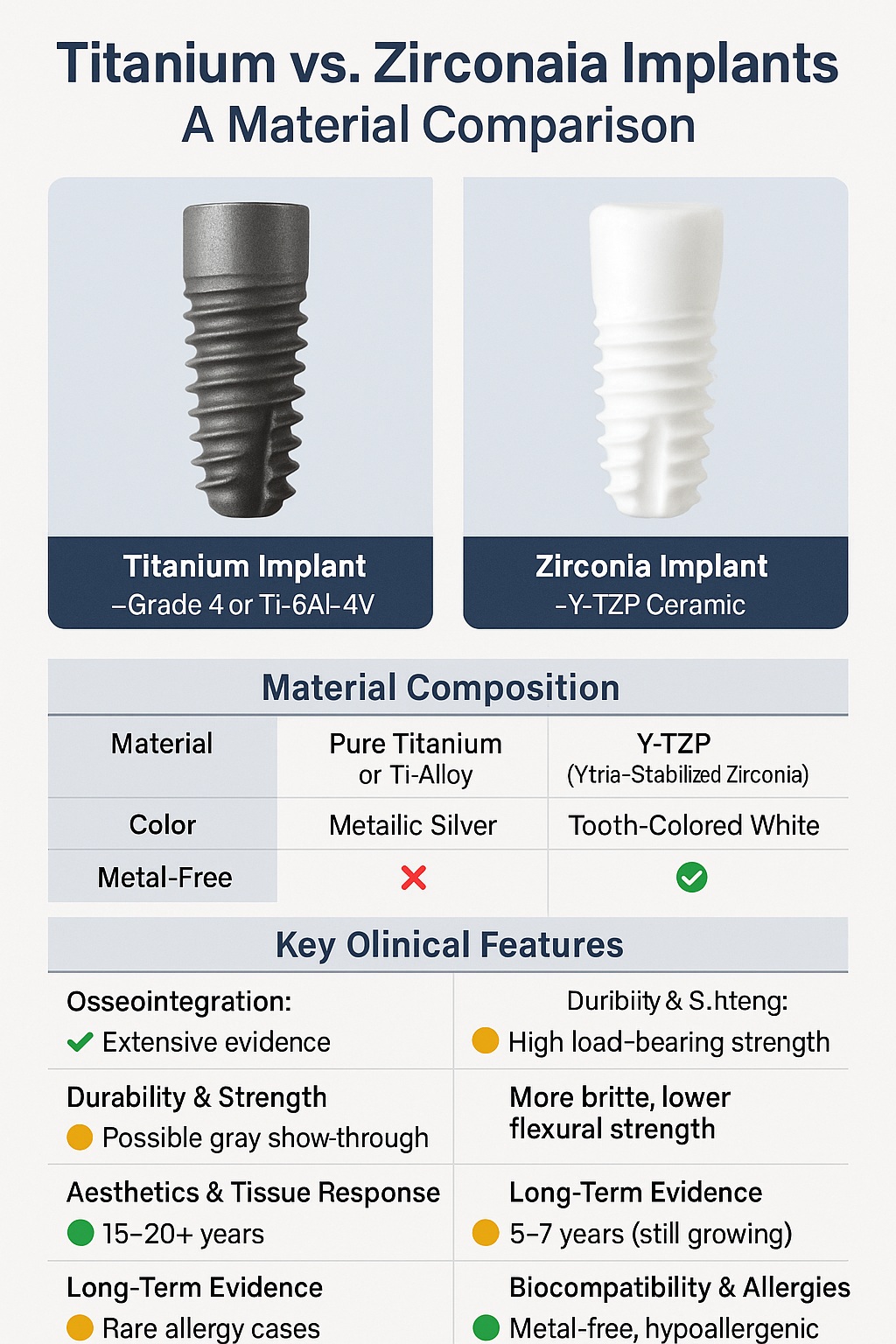
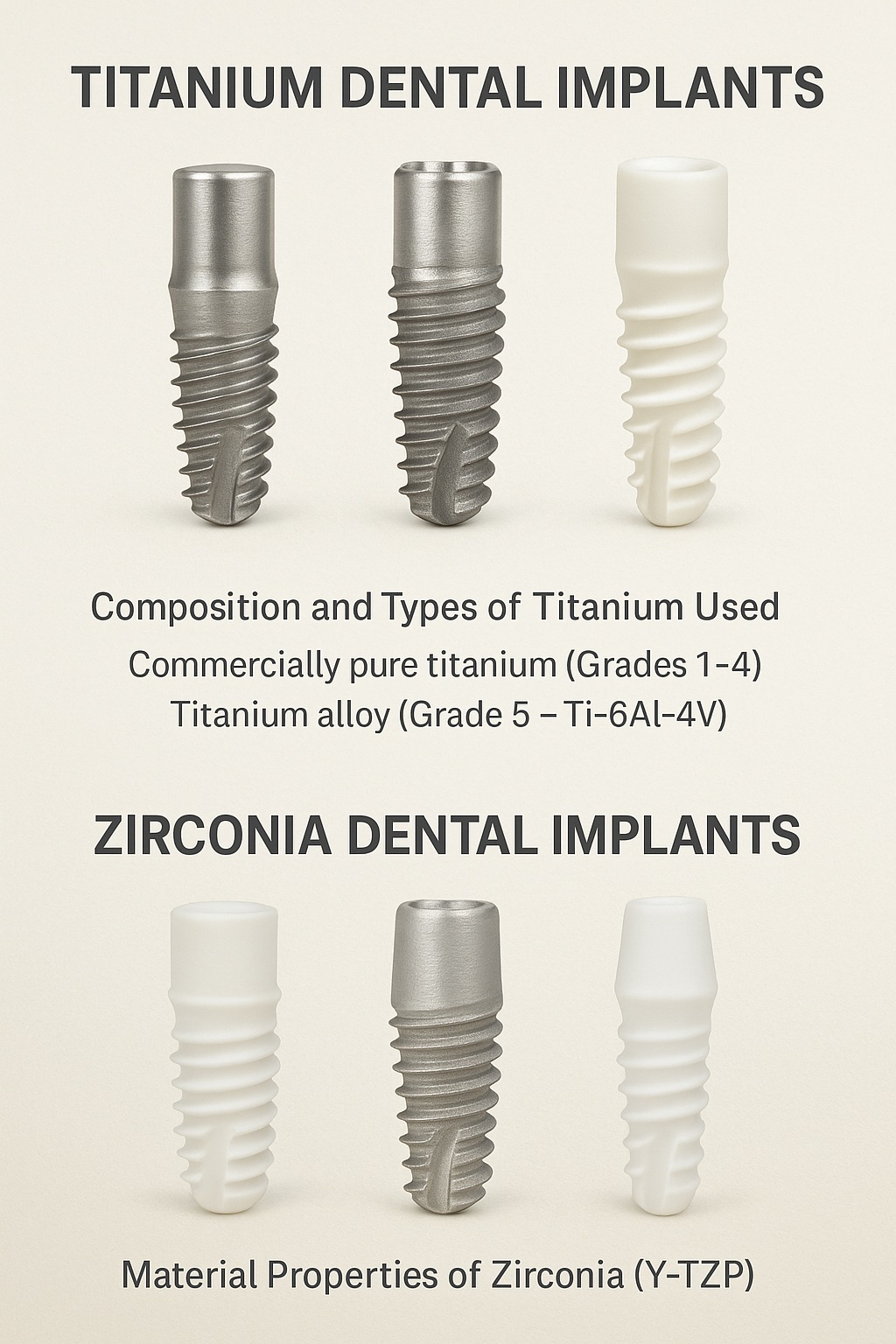
Most titanium dental implants are made from commercially pure titanium (grades 1–4) or titanium alloys, particularly Grade 5 (Ti-6Al-4V), which includes 6% aluminum and 4% vanadium. These materials are selected for their superior mechanical strength and corrosion resistance. Grade 4 titanium, with high purity and strength, is commonly used in root-form implants, while Ti-6Al-4V is often reserved for complex prosthetics due to its enhanced fatigue resistance.
Osseointegration and Biocompatibility
Titanium’s ability to fuse directly with bone — a process known as osseointegration — is a major reason for its dominance. The surface of titanium implants is often modified (e.g., SLA, anodized, or acid-etched) to enhance bone cell attachment and integration. Titanium is also bioinert, minimizing immune reactions and promoting long-term stability in the oral environment.
Long-Term Durability and Mechanical Strength
Titanium implants are highly resistant to fracture and can endure decades of functional loading. Their tensile strength and fatigue resistance make them suitable for high-stress areas like posterior jaws. Clinical data shows survival rates exceeding 95% over 10–15 years with proper placement and maintenance.
Potential Risks: Allergies and Corrosion
Although rare, hypersensitivity reactions to titanium or alloying metals (e.g., vanadium, aluminum) have been reported. Surface corrosion can occur in the presence of fluoride or acidic pH levels, potentially releasing metal ions and contributing to peri-implantitis in susceptible patients. However, such events are uncommon and usually manageable with proper patient screening.
Zirconia Dental Implants
Material Properties of Zirconia (Y-TZP)
Zirconia implants are primarily made from yttria-stabilized tetragonal zirconia polycrystal (Y-TZP), a ceramic material known for high strength and fracture toughness among ceramics. The yttria content helps maintain the tetragonal phase, which is essential for crack resistance and mechanical reliability. Unlike titanium, zirconia is metal-free and naturally white, making it aesthetically favorable for visible areas.
Biocompatibility and Soft Tissue Response
Zirconia exhibits excellent biocompatibility with low plaque accumulation and minimal inflammatory response in peri-implant tissues. Studies show favorable epithelial and connective tissue attachment, potentially reducing the risk of peri-implantitis. Its bioinert nature also eliminates the possibility of metal-related hypersensitivity or ion release.
Mechanical Strength Compared to Titanium
Although zirconia is strong for a ceramic, it is more brittle than titanium. Its resistance to flexural stress and fatigue is lower, particularly in one-piece implant designs. Innovations in material processing have improved fracture resistance, but concerns remain about long-term durability in posterior load-bearing applications.
Concerns: Fracture Risk and Limited Long-Term Data
Zirconia implants have a shorter track record than titanium, with fewer long-term clinical studies available. Fracture risk, especially in thin-diameter or one-piece systems, is a notable limitation. Additionally, modifications such as surface roughening must be carefully controlled to avoid compromising the material’s strength.
Titanium vs. Zirconia: Key Comparisons
Osseointegration Performance
Titanium remains the benchmark for osseointegration due to its well-documented success over decades. Surface treatments have been optimized to enhance bone integration and speed up healing times. Zirconia also supports osseointegration, but its surface modification options are more limited. While studies show comparable bone-to-implant contact (BIC) in the short term, long-term comparative data is still evolving.
Aesthetics and Gingival Response
Zirconia’s tooth-colored appearance provides superior aesthetics, especially in patients with thin gingival biotypes or anterior implant placements. Unlike titanium, zirconia does not cause visible gray shadows beneath the gumline. It also promotes favorable soft tissue adhesion, reducing inflammation and plaque accumulation. Titanium implants, while functionally superior in many respects, often require subgingival placement or additional soft tissue management for optimal esthetics.
Long-Term Clinical Outcomes
Titanium implants have decades of clinical data supporting survival rates of over 95% after 10–15 years. Zirconia implants are newer, with limited but promising data suggesting success rates in the 90–95% range over 5–7 years. Mechanical complications, especially fractures, are more likely with zirconia, particularly in high-load areas or under bruxism forces.
Patient Suitability Scenarios
Titanium is suitable for most patients and remains the go-to choice for full-arch, posterior, and high-load restorations. Zirconia may be preferable for patients with known metal allergies, aesthetic concerns, or requests for metal-free treatment. It is also increasingly used in holistic or biologically oriented dental practices, despite its current limitations in customization and load-bearing scenarios.
Regulatory and Safety Considerations
FDA/CE Approvals and Standards
Both titanium and zirconia dental implants are regulated medical devices subject to rigorous approval processes. Titanium implants have long-standing FDA and CE approval with well-established ISO standards (e.g., ISO 5832-2 for pure titanium and ISO 5832-3 for titanium alloys). Zirconia implants, though newer, also meet ISO and ASTM standards such as ISO 13356 for Y-TZP ceramics. However, not all zirconia systems have equivalent clinical data, so professionals should verify approvals on a product-by-product basis.
Safety Data and Clinical Evidence
Titanium implants are backed by extensive clinical research, including long-term cohort studies and systematic reviews. The safety profile is considered excellent, with low complication rates when placed and maintained properly. Zirconia implants have growing support from in vitro studies and short- to mid-term clinical trials. While safety data is generally positive, fewer long-term studies make risk assessment less certain compared to titanium.
Use Cases in Metal-Free Dentistry
For patients seeking metal-free dental solutions due to allergies, sensitivities, or personal preference, zirconia implants offer a biologically inert and esthetically neutral alternative. Their use is common in practices focused on holistic or biological dentistry. However, clinicians must be aware of the limitations in prosthetic flexibility and load tolerance, especially in complex cases or full-arch restorations.
Conclusion
Titanium and zirconia each offer distinct advantages as dental implant materials, and the choice between them should be guided by clinical requirements and patient-specific factors. Titanium remains the most reliable option, with unmatched mechanical strength, proven osseointegration, and decades of safety data. It is ideal for most surgical scenarios, especially in high-load regions or full-arch rehabilitations.
Zirconia, on the other hand, has carved out a growing role in modern implantology. Its metal-free composition, low plaque affinity, and superior aesthetics make it an attractive alternative for patients with allergies, esthetic priorities, or holistic treatment preferences. However, limitations in mechanical strength and long-term data must be weighed carefully.
For dental professionals, understanding the composition, behavior, and clinical implications of each material is key to making informed treatment decisions that align with both functional and patient-centered outcomes.