Periodontal disease is one of the leading causes of adult tooth loss, and for many people, dental implants seem like the perfect solution to restore both function and appearance. However, gum disease complicates implant treatment because healthy gums and bone are essential for long-term implant success. Patients often wonder if they can still qualify for implants after being diagnosed with periodontal disease. The answer depends on the severity of the condition, the success of treatment, and the stability of supporting tissues. Understanding the connection between gum disease and implants is the first step to making an informed decision.
Understanding Periodontal Disease
Periodontal disease, commonly known as gum disease, is a bacterial infection that affects the tissues surrounding the teeth. It begins with gingivitis, where gums become red, swollen, and prone to bleeding. If left untreated, it progresses to periodontitis, which damages the bone and ligaments that support the teeth.
One of the biggest concerns with periodontal disease is its impact on the jawbone. As the infection advances, it leads to bone loss, which directly affects the stability of teeth and future dental implants. Since implants rely on healthy bone to anchor securely, untreated gum disease can significantly reduce the chances of implant success.
Dental Implants and Their Requirements
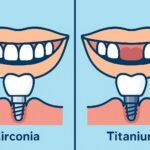
Dental implants are artificial tooth roots, usually made of titanium, placed into the jawbone to support a crown, bridge, or denture. For an implant to succeed, it must integrate firmly with the bone through a process called osseointegration. This stability depends on both bone density and healthy surrounding gum tissue.
To be considered a candidate for implants, patients generally need:
- Healthy gums free of active infection
- Adequate bone volume and density to hold the implant securely
- Good overall health since conditions like uncontrolled diabetes or smoking can reduce healing ability
- Commitment to oral hygiene to maintain implant longevity
If gum disease is present, it must be managed or eliminated before implants can be placed, as active infection undermines the healing process and increases the risk of implant failure.
Risks of Getting Implants With Gum Disease
Placing dental implants in patients with untreated or poorly managed gum disease carries significant risks. The most concerning is implant failure, which occurs when the implant does not properly fuse with the bone or becomes unstable due to infection.
Active periodontal disease increases the chance of peri-implantitis, a condition similar to gum disease but affecting implants. This leads to inflammation, bone loss around the implant, and eventual loosening or loss of the implant if untreated.
Additionally, patients with advanced gum disease often have weakened jawbone structure from bone loss, which reduces the implant’s ability to integrate successfully. Even if the implant is initially placed, the lack of strong bone support can compromise long-term stability.
Because of these risks, dentists usually require periodontal disease treatment before implant surgery can even be considered.
Treatment Before Implant Placement
For patients with periodontal disease, treatment is essential before considering dental implants. The first step usually involves scaling and root planing, a deep cleaning procedure to remove plaque and bacteria from below the gum line. In more advanced cases, periodontal surgery may be needed to reduce deep pockets and restore gum health.
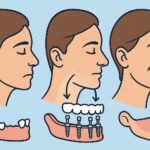
If gum disease has already caused significant bone loss, bone grafting or sinus lift procedures may be recommended to rebuild the foundation needed for implant stability. These procedures restore bone volume and increase the chances of long-term implant success.
Dentists also stress the importance of ongoing periodontal maintenance. Even after initial treatment, patients must attend regular check-ups and cleanings to ensure the infection does not return. Only once gum health and bone stability are achieved will an implant procedure be considered safe.
Long-Term Care After Implants
Patients with a history of gum disease need to be especially diligent about caring for their dental implants. Although implants cannot develop cavities, they are vulnerable to peri-implantitis, an infection similar to gum disease that damages the tissues and bone around the implant.
Daily oral hygiene is critical, including brushing twice a day, flossing or using interdental brushes, and rinsing with an antibacterial mouthwash. Regular dental checkups and professional cleanings help monitor gum health and detect any early signs of infection.
Lifestyle factors also play a role. Quitting smoking, managing conditions like diabetes, and maintaining a balanced diet all contribute to stronger gums and bone support. Patients who remain consistent with these preventive measures typically enjoy long-lasting results with their dental implants, even with a past history of periodontal disease.
Conclusion
Dental implants can be a reliable and effective solution for replacing missing teeth, but active periodontal disease poses serious challenges. Successful implant placement depends on healthy gums and strong bone support, both of which are compromised by gum disease. With proper treatment—such as gum therapy, bone grafting, and ongoing maintenance—many patients with a history of periodontal disease can still become good candidates for implants. The key is addressing gum health first and committing to long-term care to protect both natural teeth and implants.